Key takeaways:
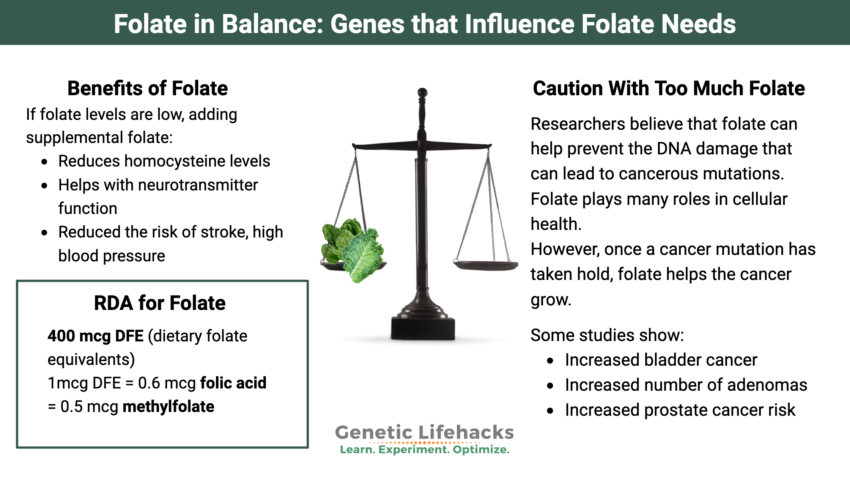
~ Balance is key with folate.
~ Having enough folate helps to protect against cancer.
~ Excess folate is linked to the growth of tumors.
What is the connection between folic acid or other folates and cancer growth?
Folate is needed for cells to replicate, which is one reason it is so important to get enough during pregnancy and why it is included in prenatal vitamins. However, rapid cellular growth is also a hallmark of many types of cancer. Tumors that grow and divide rapidly also thrive when folate is abundant. In fact, one of the first successful anti-cancer drugs was an anti-folate drug that blocks cancer cell growth by reducing folate.[ref]
Folate is often the limiting factor for DNA synthesis, which puts it in a key position to both help prevent DNA replication errors (preventing cancer) but also allowing for unchecked growth (proliferation once a cancerous mutation has developed). In addition, folate receptors are often upregulated in cancerous cells.[ref]
Thus, the balance of getting enough folate for your individual needs is important. Often, there is a focus on dramatically increasing folate levels with certain genetic variants, such as MTHFR.
Here’s an example that may surprise some of you:
The MTHFR C677T variant, which reduces the synthesis of methylfolate (active folate), is associated with a bunch of negative health outcomes. Many clinicians immediately recommend high doses of methylfolate.
But… carrying two “bad” copies of the MTHFR C677T variant also significantly reduced the risk of colon cancer and a number of other types of cancer.[ref][ref][ref][ref]
For example, a meta-analysis found that two copies of the C677T variant (AA genotype) decrease the risk of colon cancer by about 20%. Another meta-analysis found that two copies of the C677T variant (AA genotype) were protective against prostate cancer.[ref]
Here are your MTHFR variants (read the full article here on MTHFR):
| Gene | RS ID | Effect Allele | Your Genotype | Notes About Effect Allele |
|---|---|---|---|---|
| MTHFR C677T | rs1801133 | A | — | 40-70% decrease in MTHFR enzyme function (folate metabolism) |
| MTHFR A1298C | rs1801131 | G | — | 10-20% decrease in MTHFR enzyme function (folate metabolism) |
Why is the C677T variant protective against cancer?
The MTHFR C677T variant causes the enzyme to be more thermolabile and breaks down more quickly at normal body temperature. This means that there isn’t as much enzyme available to convert folate into methylfolate. The methyl groups from methylfolate are used in a bunch of ways in the body – one of which is in the synthesis of DNA during cellular replication.
How much folate is needed?
In the US and much of the world, folic acid is added to cereals, bread, enriched white rice, and anything with wheat (pizza, pop-tarts, cookies, crackers, etc). Folic acid is a synthetic form of folate that is stable in foods and during baking.
For reference, a serving of Cheerios has 235 mcg of added folic acid, a serving of bread has ~150 mcg of added folic acid, and a cup of enriched white rice has ~100 mcg of added folic acid.[ref]
Scenario:
Suppose your breakfast is 1 c. of Cheerios, lunch includes a sandwich with two slices of white bread, and your dinner is burrito (in a flour tortilla) with white rice — you would be getting more than 500 mcg of added folic acid in addition to any natural folate in the food.
The US RDA for folate is 400 mcg/day DFE. DFE stands for dietary folate equivalents (DFE). The tolerable upper limit is set at 1,000 mcg/day from supplements or fortification (limit for adults, lower for teens and children).[ref]
What are dietary folate equivalents?
The DFE refers to how supplemental forms of folate equate to folate that you get from food. Food folate is equal to one dietary folate equivalent (DFE), which makes sense. Folic acid and methylfolate are more available to be absorbed in the intestines.
Here’s how they are factored:
1 DFE = 1mcg of folate from food = 0.6 mcg folic acid or 0.5 methylfolate
Back to my scenario: If you eat breakfast cereal, a sandwich with two slices of enriched bread, and a burrito with rice for dinner (totaling at least 500 mcg of folic acid), you end up with 833 mcg DFE just from added folic acid.
If you find out about a MTHFR variant and decide that you need a methylfolate supplement, the most common supplement dosage you’ll find is 1 mg. (1 mg is 1,000 mcg, equivalent to 2,000 mcg DFE.)
Folate is important in preventing cancer, but…
Researchers believe that folic acid and other forms of folate help prevent the DNA damage that can lead to cancerous mutations. Folate plays many roles in cellular health.
But the flip side is that once a cancer mutation has taken hold, folate helps the cancer grow. Folate is essential for cell growth, and cancer cells use a lot of folate.[ref]
Let’s take a look at studies that raise questions about folate increasing cancer risk or growth:
A randomized, placebo-controlled trial evaluated the effect of 1 mg/day (1,000 mcg/day) of folic acid in preventing colorectal cancer in a group of 987 adults. Participants were followed for 6 to 8 years, with colonoscopies performed to determine the prevalence of colorectal adenomas. While there was no increase in the risk of colorectal adenomas after the first three years, follow-up 3-5 years later showed that the folic acid group had an increased risk of recurrence of advanced adenomas with high malignant potential (67% increased relative risk).[ref]
In bladder cancer patients, a 5-year prospective study showed that both moderate and high folic acid intake significantly increased the risk of recurrence by 65-80%.[ref]
Of note here, both the bladder and colorectal cancer trials were in adults who were likely at a higher cancer risk.
Does adding other B vitamins change things?
The overall increased risk of cancer was assessed in a long-term follow-up study of an osteoporosis prevention trial involving 2,524 adults who took folic acid (400 µg) and vitamin B12 (500 µg) compared with a placebo. The follow-up showed that those who were randomized to the folic acid/B12 group had a 13% increased relative risk of overall cancer and a 77% increased relative risk of colorectal cancer.[ref]
TL;DR: In people who are at a higher risk of cancer (e.g. older or with prior cancers), folic acid increases the incidence of cancer, especially colon cancer.
Is unmetabolized folic acid the problem, or is it the increase in active folate (methylfolate)?
A study that looked at folic acid, unmetabolized folic acid, and methylfolate levels found that higher levels of methylfolate (5-methyltetrahydrofolate) were statistically associated with a 58% increased relative risk of advanced or multiple adenomas (benign tumors). The results also showed that unmetabolized folic acid was not statistically associated with adenomas.[ref]
(For more on unmetabolized folic acid, see my article on the DHFR gene.)
TL;DR Research shows that both methylfolate and folic acid could increase tumor risk.
What about prenatal exposure to folic acid?
A large study of children born between 1997 and 2017 looked at the effects on children whose mothers had taken high doses of folic acid while pregnant. The researchers defined high doses of folic acid as 1,000 mcg (most prenatal vitamins contain 800 mcg). The results showed an almost threefold increased relative risk of childhood cancer in children whose mothers had epilepsy and took 1 mg of folic acid. However, there was no increased risk of cancer in children whose mothers had epilepsy but didn’t take folic acid. In the group of mothers without epilepsy who took 1 mg of folic acid, there was a smaller (~10%) increased relative risk of childhood cancer.[ref]
What about dietary folate?
This study surprised me, and I’m still not sure what to make of it. A prospective study looked at dietary folate and skin cancer in middle-aged adults. The median follow-up time for the study was 12 years. The results showed that higher dietary folate intake and higher erythrocyte folate concentration were associated with an increased risk of skin cancer. The increase in relative risk was 79% for people in the top third of dietary folate intake compared to the bottom third. The study was conducted in France from 1994-2002, and there was no fortification of foods with folic acid there.[ref]
TL;DR One study done prior to folic acid fortification showed that higher dietary folate was associated with increased skin cancer risk.
Folate is also good for you, in many ways:
I don’t want to give anyone the impression that folic acid and/or methylfolate are all bad. Many studies show the benefits of dietary folate and supplemental folic acid. (There aren’t very many placebo-controlled clinical trials using methylfolate.) Studies also show that eating folate-rich foods is good for your health in multiple ways.
- Reducing homocysteine levels with folate has benefits for both heart health and cognitive function. In people with both high homocysteine levels and high blood pressure, one study found that 800 mcg of folic acid helped lower blood pressure and homocysteine levels[ref]
- A study of adults aged 50-70 years with high homocysteine levels (≥13 µmol/L) showed that 800 mcg of folic acid for three years had a beneficial effect on cognitive test scores, but only for the participants who also had low omega-3 levels.[ref]
- There are studies using methylfolate for psychiatric symptoms that show positive results that are statistically significant at high doses.[ref][ref]
The key to evaluating trials is to look at what outcomes are being tracked (e.g. cancer vs. heart health) and the age of the participants (young vs. old). Additionally, look at the amount of folate used in the study. Many studies show a positive benefit in cancer prevention for getting adequate folate (e.g. the RDA) in comparison to being deficient in folate.[ref]
Nitrates and folic acid:
A recent study and subsequent recall (in Canada) of some brands of folic acid supplements showed that some of the supplements contain low levels of N-nitroso-folic acid, which is carcinogenic. N-Nitroso folic acid can be produced when folic acid reacts with sodium nitrate in a solution.[ref]
When would you have folic acid reacting with nitrates or nitrites in solution (other than in manufacturing)? Well, when nitrites are in the drinking water…
A study published in 2013 looked at the combination of folate intake, nitrate intake from public water sources, and breast cancer risk. The study included more than 20,000 women in Iowa with survey information on dietary folate intake from 1986. The study then followed the women (ages 55-69) for cancer incidence for a number of years.
Dietary nitrates, nitrites, and nitrites from drinking water were not associated with increased breast cancer in women with a normal or low folate intake. However, there was a 40% increased relative risk of breast cancer in women with higher nitrate levels in their water who also consumed more than 400 mcg/day of folate.[ref] Another study on Korean women found a similar result.[ref]
Conclusion:
I don’t have all the answers here, but I worry that some people are going overboard on folate and may not understand the risks vs. benefits. I’ve seen so many articles and podcasts recommending methylfolate supplements at relatively high doses for anyone with an MTHFR variant, but I don’t see much on the possible negative consequences.
Talk with your doctor, of course, if you have questions on how much folate (folic acid, methyl folate, folinic acid) you take. There may be a specific reason for the recommendation for your individual case. Some medications interact with folate and necessitate taking higher doses.
The research clearly shows a tradeoff — more is not always better when it comes to folate, folic acid, and methylfolate. Please read through the studies for yourself.
To optimize folate, I think individuals need to take into account their age, homocysteine levels, cancer risk factors, family history of cancer, genetic variants in the folate pathway, and how much nitrite is in their water and diet. Plus, there are probably other environmental factors (like nitrates in groundwater) that I don’t know about!
If you are worried about excess folate but want to support cellular health with an MTHFR variant, consider creatine. About 40% of methyl groups go towards the synthesis of creatine, so supplementing with creating helps to take the burden off the system. You can read more in the MTHFR article and the Creatine article. Also, keep in mind that you could cut a 1 mg (1,000 mcg) methylfolate table in half or in fourths to dial in a lower dose.
Related articles and topics:
About the Author:
Debbie Moon is the founder of Genetic Lifehacks. Fascinated by the connections between genes, diet, and health, her goal is to help you understand how to apply genetics to your diet and lifestyle decisions. Debbie has a BS in engineering from Colorado School of Mines and an MSc in biological sciences from Clemson University. Debbie combines an engineering mindset with a biological systems approach to help you understand how genetic differences impact your optimal health.